Understanding Piriformis Syndrome: Insights & Physiotherapy Interventions
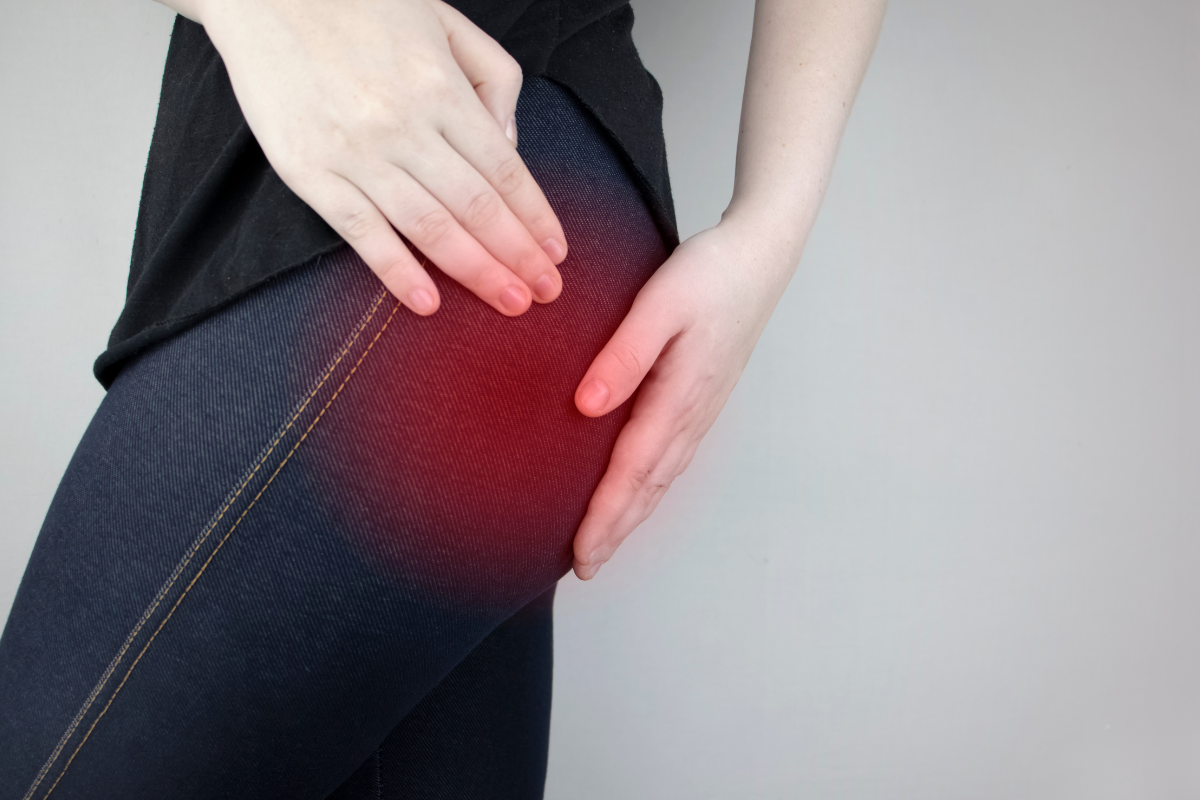
Piriformis syndrome is a condition characterised by pain in the buttock region, often radiating down the leg. It occurs when the piriformis muscle, located deep in the gluteal region, irritates the sciatic nerve. This syndrome can significantly affect mobility and quality of life. In this blog, we will explore the causes, symptoms, diagnosis, and effective physiotherapy interventions for managing piriformis syndrome.
What is Piriformis Syndrome?
Piriformis syndrome is often described as a neuromuscular disorder that results from the compression or irritation of the sciatic nerve by the piriformis muscle. This muscle is responsible for the external rotation and abduction of the hip. When it becomes tight or spasms, it can lead to pain and discomfort, mimicking sciatica (Cameron & Swanson, 2019).
Causes:
Various factors can contribute to the development of piriformis syndrome, including:
Muscle Tightness: Prolonged sitting, overuse, or lack of flexibility in the hip muscles can lead to tightness in the piriformis.
Injury:
Trauma to the hip or buttock region can cause inflammation or spasms of the piriformis muscle.
Anatomical Variations: Some individuals may have anatomical variations that predispose them to nerve compression.
Repetitive Activities: Activities such as running, cycling, or prolonged sitting can exacerbate symptoms
(Kumar et al., 2020).
Symptoms:
The hallmark symptom of piriformis syndrome is pain in the buttock, which may radiate along the path of the sciatic nerve down the leg. Other symptoms may include:
- Numbness or tingling in the buttock or leg
- Pain that worsens with prolonged sitting or standing
- Discomfort during activities that involve hip movement, such as climbing stairs or squatting (Bahr et al., 2017).
Diagnosis:
Diagnosing piriformis syndrome involves a thorough history and physical examination. Key steps include:
Clinical History: Gathering information on the onset, duration, and nature of the pain.
Physical Examination: Assessing range of motion, strength, and tenderness in the hip and buttock region.
Special Tests: Tests such as the Piriformis Test or Freiberg’s Test can help identify piriformis syndrome by reproducing symptoms during specific movements
(Cameron & Swanson, 2019).
Imaging studies, such as MRI or ultrasound, may be utilised in complex cases to rule out other conditions.

Physiotherapy Interventions
Physiotherapy plays a crucial role in the management of piriformis syndrome. Key interventions include:
1. Manual Therapy
Manual therapy techniques, including soft tissue mobilisation and joint manipulation, can help alleviate muscle tightness and improve mobility in the hip region
(Bahr et al., 2017).
2. Exercises That Stretch & Strengthen Muscles
- Stretching the piriformis and surrounding muscles is essential for reducing tension.
- Strengthening the hip and gluteal muscles can help support proper biomechanics.
3. Postural Education and Ergonomics
Educating patients about proper posture, especially during prolonged sitting or repetitive activities, can prevent exacerbation of symptoms. Ergonomic adjustments at work or during sports can also be beneficial.
Conclusion
Piriformis syndrome can be a debilitating condition affecting many individuals, particularly those engaged in activities that strain the hip and lower back. Physiotherapy offers a comprehensive approach to managing this syndrome, focusing on pain relief, improved mobility, and restoring function. By employing a combination of manual therapy, targeted exercises, and education, physiotherapists can help patients regain their quality of life and return to their daily activities.
It must also be noted that Piriformis Syndrome can often be misdiagnosed and if the exercises prescribed for this make your symptoms worse, please stop and see a Specialist Physio.
Chelmsford Physio
Riverside Leisure Centre, Victoria Rd, Chelmsford CM1 1FG
GET IN TOUCH
Chelmsford Physio
Riverside Ice and Leisure Centre,
Victoria Road
Chelmsford
CM1 1FG
Tel:
01245 895410
Email:
hello@chelmsfordphysio.co.uk
STAY CONNECTED
Join our newsletter and find out more
Contact Us
Thank you for signing up!
Please try again later