What does Arthritis mean to you?

The term Arthritis can often be misunderstood. When we ask a patient about arthritis in clinic during the assessment part of the appointment, we are asking for a specific reason, but often a patient will look confused or unsure. We will hear patients tell us about being diagnosed with arthritis by their GP, this can be scary, causing fear and avoidance of exercise.
We will also hear patients, who have self diagnosed themselves with having arthritis or sometimes “rheumatism”. Therefore this blog will try to help you understand the term Arthritis and therefore help towards managing the symptoms it can cause.
To keep it simple here we will discuss the 2 main forms of arthritis
1. Osteoarthritis (OA)
2. Rheumatoid Arthritis (RA)
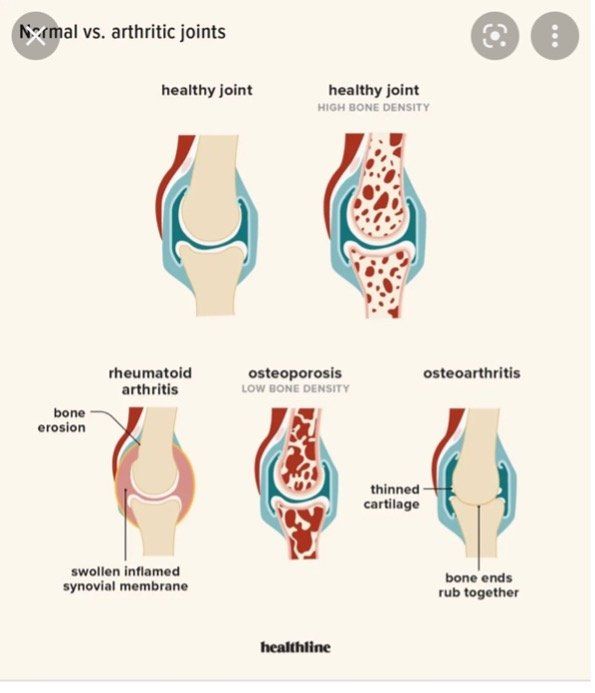
Osteoarthritis (OA)
This is the most common chronic condition of the joints. OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe.
OA affects 8 million people in the UK (Arthritis Research UK). We often talk about OA being similar to grey hair and wrinkles – it’s describing an aging process which may or may not include pain.
OA is a condition whereby the surfaces of your joints become altered. Cartilage at the end of the joints become roughed and thin. As with many injuries, imaging for OA can sometimes be helpful. However, you can look at results from a scan and think the patient is bound to have pain, swelling and struggle with daily activity. However, in reality they were actually doing really well. Essentially there is a poor relationship between findings on x-ray and MRI, versus functional pain and problems with daily activities.
In clinic we see patients every day with OA, with a spectrum of symptoms. These symptoms can often be disproportional to the findings on an Xray or scan.
There are some key things that we can do to improve and settle symptoms and work on longer term strategies to achieve help too.
Some of the key areas physiotherapy can help with are
· Provide the best information, education and advice
· Improving range of motion at the joints
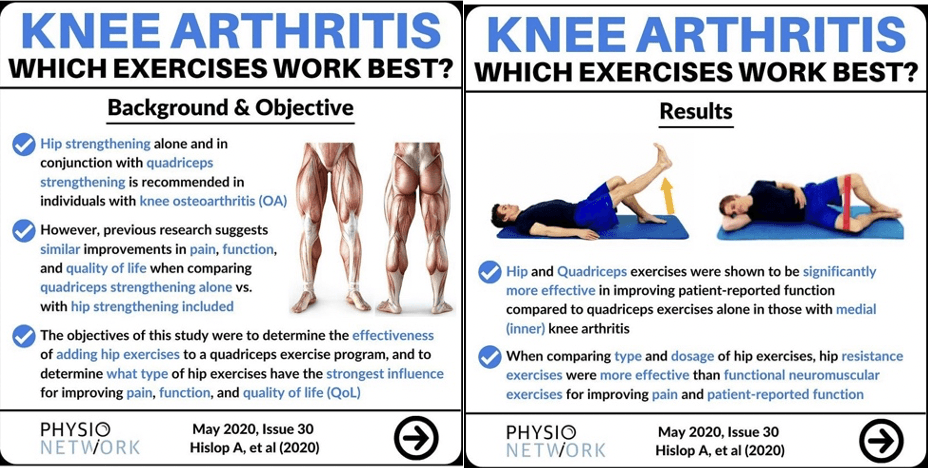
· improving muscle strength around the areas
· Cardiovascular fitness
· Weight management
The National Institute for Health and Clinical Excellence (NICE) recently reviewed its advice on OA. They recommended access to appropriate information, activity and exercise. If anyone is overweight, they should be offered advice to lose weight. Looking at the exercise, this should include local strengthening and general cardiovascular exercise. They also advocated the use of heat/ice therapy, manual therapy and specific strengthening exercises.
There are so many variable when it comes to an exercise plan/program, it should also be bespoke to the individual, rather than a one size fits all.
It depends on your individual capabilities, your personal circumstances and what you enjoy. We see many people at Chelmsford Physio who want guidance to ensure they get the most out of their exercise.
Rheumatoid arthritis (RA)
This is a completely different type of arthritis. RA is a systemic autoimmune disease characterized by inflammatory arthritis and can involve many other features including
· Waking during the night and morning stiffness >30mins
· IBS
· Fatigue, weight loss, night sweats
· Dactylitis ( swollen finger )
· Iritis (inflammation of the eyes pupil, Iris)
· Psoriasis
· Anaemia (reduced red blood cells
· Enthesitis (inflammation of the ligament/tendon attachment to bone)\
So you can see why we ask some of the questions we do within the assessment part of your session. These clues are often very helpful in detecting and diagnosing some of the various types of inflammatory arthritis we see in clinic including
· AS ( Axial Spondyloarthritis)
· Reactive Arthritis
· Psoriatic Arthritis
· PMR (Polymyalgia Rheumatica)
· Gout
· Hypermobility

Diagnostic delay is an ongoing challenge and often these inflammatory type arthritis can be missed for years, due to a mixed presentation and intermittent symptoms. The current research suggests a mean average of 8-9yrs delay, between symptom onset of AS and formal diagnosis in the UK. The key is to see a physiotherapist or specialist who has a high awareness of the clues and symptoms associated with the various inflammatory arthritis.
These may all be a disease of the joints but they also have systemic repercussions. The management is ideally done by an interprofessional team that includes a GP and a rheumatologist, so onward referral for appropriate investigations at the earliest detection is key.
Further investigations may include
· Blood tests
· Xrays
· MRI
· US scan
Living with arthritis can be different from person to person, and symptoms can vary from day to day. Treatment and management options vary with the type of arthritis, its severity and the parts of the body affected.
There is no cure for arthritis. Management options can include medical treatment and medication, physiotherapy, exercise and self-management techniques.
If you have any questions or concerns regarding arthritis or would like to speak to one of our physiotherapists, please email hello@chelmsfordphysio.co.uk
https://www.physio-pedia.com/Osteoarthritis
https://rheumatology.physio/mini-blog-screendem